Topic
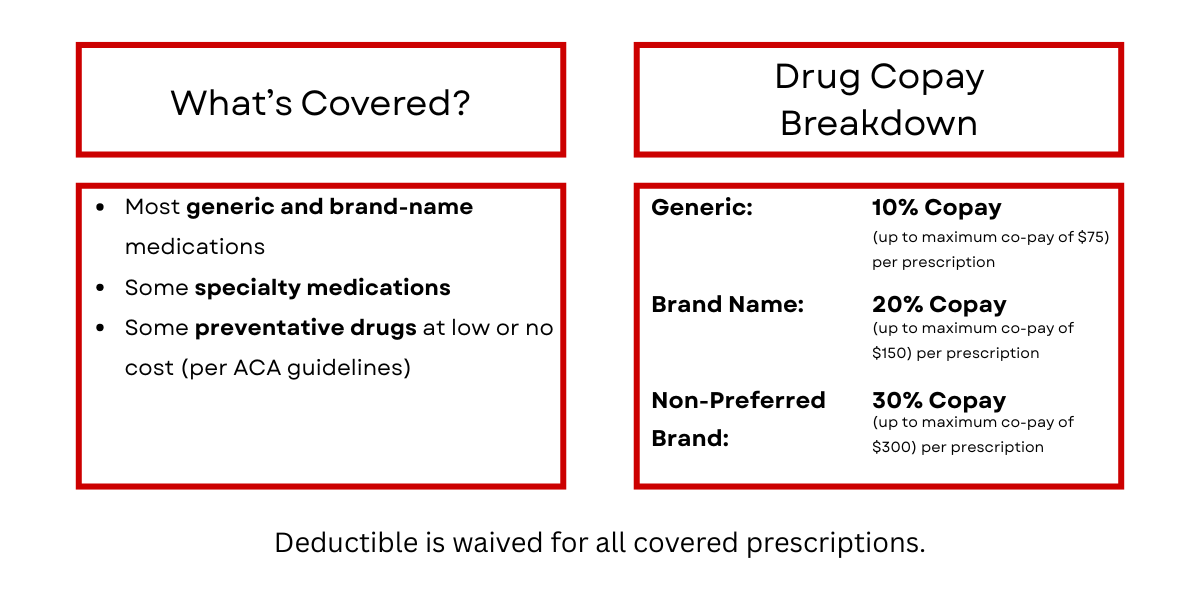
MSB Employee Benefit: Pharmacy Coverage

Prescription Drug Benefit is administered by CVS Caremark.
How to Use Your Benefits
- Present your insurance card at the pharmacy.
-
Use in-network pharmacies for the best prices.
-
Consider mail-order for 90-day supplies (if available).
-
Choose generics when possible—they cost less and work the same.
Formulary (Drug List)
Check the formulary to see if your medication is covered. A formulary is a summary of which medications are covered, which are not and which medications can be used in place of non-covered medications.
Note: Not all drugs on the list are covered for all diagnoses. Coverage depends on your condition and treatment plan.

Prior Authorization & Step Therapy
Some drugs may require:
-
Prior authorization (approval before filling)
-
Step therapy (trying a lower-cost drug first)
-
Quantity limits
Your doctor can help submit these requests.
Need Help?
-
Pharmacy Benefit Manager (PBM): call 1-866-818-6911 or visit www.caremark.com.
-
HR/Benefits Team: Nicole Kantrowitz, Healthcare Concierge (907) 861-8503
Contact
Nicole Kantrowitz
Healthcare Concierge
Contact
Nicole Kantrowitz
Healthcare Concierge
